07 Apr 2016 [98] Does SPRINT change our approach to blood pressure targets?
 Therapeutics Letter #821 summarized evidence from the Cochrane systematic review, Treatment blood pressure targets for hypertension.2 The Cochrane review was based on the 7 randomized controlled trials (RCTs) designed to test treatment targets that were available as of October 2008. The conclusion was that “Treating patients to lower than standard blood pressure (BP) targets (≤ 140-160/90-100 mmHg) does not reduce mortality or morbidity.”
Therapeutics Letter #821 summarized evidence from the Cochrane systematic review, Treatment blood pressure targets for hypertension.2 The Cochrane review was based on the 7 randomized controlled trials (RCTs) designed to test treatment targets that were available as of October 2008. The conclusion was that “Treating patients to lower than standard blood pressure (BP) targets (≤ 140-160/90-100 mmHg) does not reduce mortality or morbidity.”
SPRINT
In September 2015, Systolic blood PRessure INtervention Trial (SPRINT) added a new trial that studied BP targets. It was stopped early for benefit. Results were published in November 2015.3 SPRINT randomly assigned 9361 persons with a systolic BP of 130 mmHg or higher and an increased cardiovascular risk (but without diabetes or prior stroke) to a low systolic BP target of < 120 mmHg or a standard target of < 140 mmHg. SPRINT was an open label trial conducted at 102 sites. The average achieved BP at one year in the low BP target group was 121/69 versus 136/76 mmHg in the standard BP target group. The average number of antihypertensive drugs in the low BP target group was 2.8, vs. 1.8 in the standard BP target group.
Benefits
After an average duration of 3.3 years, the primary outcome (a composite of myocardial infarction, acute coronary syndrome, stroke, acute decompensated heart failure, or death from cardiovascular causes) was decreased in the low BP target group at 5.2%, vs. 6.8% in the standard BP target group, RR 0.76 [0.65, 0.90], ARR 1.6%, NNT 63 for 3.3 years.
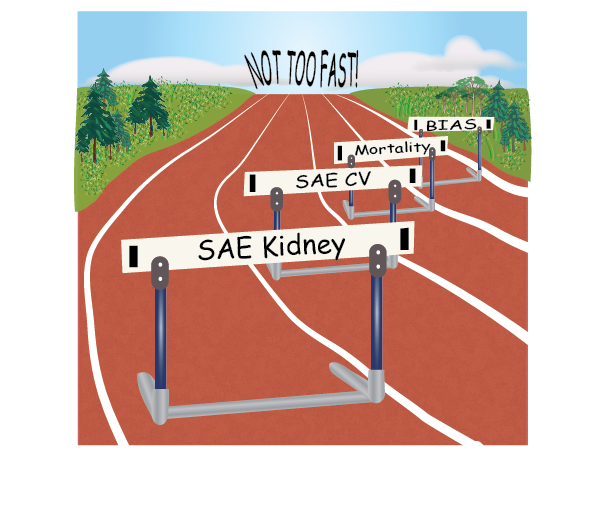
Harms
Specific serious adverse events classified as possibly or definitely related to the intervention were increased in the low BP target group, 4.7%, vs. 2.5% in the standard BP target group, RR 1.87 [1.50, 2.33] ARI 2.2%, NNTH 46 for 3.3 years. This was due mainly to a 1.2% absolute increase in acute kidney injury or acute renal failure in the low BP target group.
Overall effect
Total serious adverse events were appropriately defined as fatal or life-threatening events resulting in clinically significant or persistent disability, or events that required or prolonged a hospitalization. The number of people with one or more serious adverse events was numerically greater in the low BP target group at 38.3% vs. 37.1% in the standard BP target group, RR 1.03 [0.98, 1.09]. However, deaths were significantly lower in the low BP target group at 3.3%, vs. 4.5% in the standard BP target group, RR 0.74 [0.60, 0.91], ARR 1.2%. These two findings are hard to reconcile, insofar as this means the number of people with non-fatal serious adverse events was significantly greater in the low BP target group, at 35.0% vs. 32.6% in the standard BP target group, RR 1.07 [1.02, 1.14], ARI 2.4%.
Risk of bias
Because of the BP target design, investigators could not be blinded to treatment group. This results in a high risk of performance and detection bias. Performance bias means the people caring for the patients treat the lower BP target group preferentially. Detection bias means investigators ascertain the outcomes in favour of the lower target group. Evidence of such bias in SPRINT is that the observed mean BP difference between the two groups of 15/7 mmHg is much greater than expected from a mean difference of one antihypertensive drug (2.8 vs. 1.8) between the target groups. The average BP reduction produced by a single antihypertensive drug has been studied extensively and estimated at about 8/5 mmHg.4-7
Stopping the trial early for benefit also adds additional risk of bias in favour of the lower BP target.8 This action would tend to exaggerate the benefits and underestimate the harms outlined above. We judge that the outcome least susceptible to bias is the total serious adverse events (SAE), because investigators presently do not recognize this outcome as an important way to assess the benefits and harms of an intervention.
Clinical implications of SPRINT
Most of the editorials and commentaries about the SPRINT trial have given it a positive spin and recommended that target BPs should be lower as a result of this trial. These commentaries have ignored the finding that individuals experiencing at least one serious adverse event were numerically increased in the low BP target group. None of these commentaries have situated SPRINT into the totality of available evidence on BP lowering targets.
Systematic review
The relevant Cochrane review has the objective: To determine if there is a reduction in total mortality and morbidity associated with treatment of blood pressure to “lower targets” (≤ 135/85 mmHg) as compared with “standard targets” (≤ 140-160/90-100 mmHg) in the management of patients with elevated arterial blood pressure. First published in 2009, it is now being updated. In addition to SPRINT, two large trials, ACCORD and SPS3 have been added to the review.9,10 In the updated review, mortality data from 11 RCTs (N = 38,584) indicate that lower targets do not reduce total mortality, RR 0.95 [0.86, 1.05]. Furthermore this analysis demonstrates that the mortality data from SPRINT are discordant with the rest of the trials. In a sensitivity analysis with SPRINT removed, the RR for total mortality in the remaining 10 RCTs (N = 29,223) increased to RR 1.03 [0. 92, 1.05]. Unfortunately, total serious adverse events were reported in only 3 of the 11 RCTs. In these 3 RCTs (N = 14,432), total serious adverse events were not decreased in the low BP target group, RR 1.03 [0.99, 1.08].
Other non-Cochrane systematic reviews
Systematic reviews that combine all RCTs comparing more intensive with less intensive BP therapy11,12 are misleading and should not be used as evidence in favour of lower targets. These reviews include trials with markedly different targets, for example, a trial comparing a BP target of < 150/85 with < 180/105 mmHg.13
Conclusions
- At the present time, lower BP targets (≤ 135/85 mmHg) have not been demonstrated to reduce mortality or total serious adverse events as compared with standard BP targets (≤ 140-160/90-100 mmHg).
- Careful analysis of the SPRINT trial reveals that benefits of a lower blood pressure target in high-risk nondiabetic people do not outweigh harms.
- Critical appraisal of systematic reviews and clinical trial reports often leads to interpretation and conclusions different from initial impressions.
Abbreviations:
BP = Blood pressure
RCT = Randomized control trial
SAE = Serious adverse event
RR = Relative risk, risk ratio
ARR = Absolute risk reduction
ARI = Absolute risk increase
NNT = Number needed to treat to prevent one event
NNTH = Number needed to treat to cause one harmful event
References
- Therapeutics Initiative. Clinical hypertension pearls from the Cochrane Library. Therapeutics Letter. Jul-Aug, 2011; 82:1-2. [Letter #82]
- Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No.: CD004349. DOI: 10.1002/14651858.CD004349.pub2.
- SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Eng J Med. 2015; 373: 2103-16. DOI: 10.1056/NEJMoa1511939.
- Heran BS, Wong MMY, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD003823. DOI: 10.1002/14651858.CD003823.pub2.
- Heran BS, Wong MMY, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin receptor blockers for primary hypertension. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD003822. DOI: 10.1002/14651858.CD003822.pub2.
- Wong GWK, Wright JM. Blood pressure lowering efficacy of nonselective beta-blockers for primary hypertension. Cochrane Database of Systematic Reviews 2014 , Issue 2. Art. No .: CD007452. DOI: 10.1002/14651858.CD007452.pub2.
- Musini VM, Nazer M, Bassett K, Wright JM. Blood pressure lowering efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane Database of Systematic Reviews 2014, Issue 5. Art. No .: CD003824. DOI: 10.1002/14651858.CD003824.pub2.
- Bassler D, Briel M, Montori VM, et al. Stopping randomized trials early for benefit and estimation of treatment effects: systematic review and meta-regression analysis. JAMA. 2010;303(12):1180-87. DOI: 10.1001/jama.2010.310.
- ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Eng J Med. 2010;362(17):1575-85. DOI: 10.1056/NEJMoa1001286.
- SPS3 Study Group. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet 2013;382(9891):507-15. DOI: 10.1016/S0140-6736(13)60852-1.
- Lv JC, Neal B, Ehteshami P, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS Med 2012; 9(8):e1001293. DOI: 10.1371/journal.pmed.1001293.
- Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 2016;3 87(10017 ):435-43. DOI: 10.1371/journal.pmed.1001293.
- UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. Brit Med J. 1998; 317(7160):703-13. DOI: 10.1136/bmj.317.7160.703.





Ronald H Estey
Posted at 21:04h, 07 AprilThank you so much for this review. I have been waiting for a critical review of SPRINT ever since it hit our local newspaper!
Chris Krause
Posted at 12:44h, 08 AprilExcellent summary.
I think the most important point made here is: “the mortality data from SPRINT are discordant with the rest of the trials.” We should not believe that this trial is correct simply because it is positive – if anything, stopping for benefit is more likely to falsely inflate the effect and increases bias, as you point out.
It is up to the investigators to explain why we should believe their trial is correct and the rest of the existing evidence is all wrong – something which I don’t think is possible given our current knowledge. If a different group re-produced SPRINT, naturally that would give their hypothesis more credence.
Gerald Tevaarwerk
Posted at 08:38h, 29 AugustApart from the danger of bias having reduced the strength of the evidence these large studies show “statistically significant” differences in outcomes. What is missing is whether those differences are “clinically important”, especially as applied to an individual patient. The studies are about large groups (“samples”) of patients that differ statistically 19 out of 20 times but without specifying how “clinically important” those differences are to the groups, let alone to an individual patient. In clinical research one should first define what would be considered “clinically important” and then determine what it takes to achieve those goals. The nature of the statistical analyses used is such that if enough patients are studied even the smallest clinical difference can be shown to be “statistically significant” 19 out of 20 times, but is it “clinically important”? That is, to the group (“sample”) in the trial. An illustrative way of expressing those results is ‘how many patients need to be treated to obtain one such “clinically important” outcome’, known as “Numbers Needed to be Treated”. Stated as “one subject out of xxx did not have a clinically important negative outcome”, there is no way of identifying which individual patient would be so lucky! Nor can it be concluded that all participants in such a treatment would have an equal amount of reduction in their risk of having that particular clinically important negative outcome. We need to find a better way of how to express the reduction in risk of a “clinically important” negative outcome in individual patients. That, after all, is what we deal with in our practice.